This blog post was written by Victoria L. Freeman, Ph.D., CHFS, CMH, CBC, and reviewed by Lauren Ameling, DC, BCND.
Have you ever felt your stomach tighten when anxious about something or felt "butterflies" before speaking in public? These two scenarios are examples of the link between our thoughts, beliefs, attitudes, and physical health, commonly known as the mind-body connection. As holistic health practitioners, we know that our mental and emotional health is interwoven with our physical health; indeed, each affects the other. Spiritual health is also part of the mix when looking at this connection through a truly holistic lens, but for this blog, we'll focus on the mind-body relationship.
Practices such as meditation, breathing techniques, Tai Chi, qigong, or yoga take advantage of the interaction between mind and body with the goal of reducing stress and promoting health. Plenty of research supports the effectiveness of such practices, but how do they work? That is, how do these mind-body practices help effectively support individuals with conditions such as anxiety and depression, coronary artery disease, chronic pain from fibromyalgia or osteoarthritis, multiple gastrointestinal challenges like irritable bowel syndrome or ulcerative colitis, hypertension, and insomnia? When you study this further, you find that reversing the effects of chronic stress by decreasing levels of stress hormones is certainly a primary part of the answer. But, the mechanism through which your body responds to mind-body practices to accomplish this reduction in the detrimental levels and effects of stress hormones is carried out by the vagus nerve, your body's longest neural superhighway that transports messages from your brain out into your body and from your body back to your brain. You might say the vagus nerve is the mind-body connection.
This remarkable part of your nervous system exerts a powerful effect on multiple aspects of health, including mediating the effects of stress. So, let's look closer at the vagus nerve and its importance from a holistic health perspective.
The Vagus Nerve: What You Need to Know About It and Why It Matters
What is the Vagus Nerve?
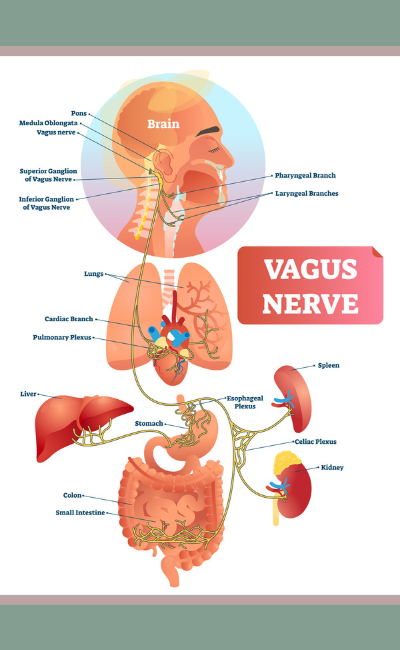 The vagus nerve is the tenth of twelve pairs of cranial nerves. From its origin in the brainstem, it extends through the neck and thorax, down into the abdomen, and terminates in part of the colon. Along the way, this "wandering nerve" (the word "vagus" is Latin for the word "wandering") is responsible for a wide variety of physiological actions such as swallowing and vocalization, slowing the heart rate, immune response, digestion, and even mood. Its action is a neural mix, meaning it has both motor (efferent) and sensory (afferent) nerve fibers. Sensory neurons carry information from the sensory organs to the central nervous system (CNS), and motor neurons take information from the CNS to muscles and glands.4 Even though historically the vagus nerve has been recognized for its efferent actions, we now know that perhaps its most important health functions are as the "brakes" for the sympathetic (stress-promoting) nervous system and the collection of sensory information from the internal organs such as your gut, liver, heart, and lungs to send feedback messages to the brain.
The vagus nerve is the tenth of twelve pairs of cranial nerves. From its origin in the brainstem, it extends through the neck and thorax, down into the abdomen, and terminates in part of the colon. Along the way, this "wandering nerve" (the word "vagus" is Latin for the word "wandering") is responsible for a wide variety of physiological actions such as swallowing and vocalization, slowing the heart rate, immune response, digestion, and even mood. Its action is a neural mix, meaning it has both motor (efferent) and sensory (afferent) nerve fibers. Sensory neurons carry information from the sensory organs to the central nervous system (CNS), and motor neurons take information from the CNS to muscles and glands.4 Even though historically the vagus nerve has been recognized for its efferent actions, we now know that perhaps its most important health functions are as the "brakes" for the sympathetic (stress-promoting) nervous system and the collection of sensory information from the internal organs such as your gut, liver, heart, and lungs to send feedback messages to the brain.
The vagus nerve is the primary component of the parasympathetic nervous system (PNS), also known as the "rest and digest" or "growth and healing" part of the nervous system. The PNS de-stresses or calms things down, whereas the sympathetic nervous system (SNS) is what revs things up. For example, our survival "fight or flight" response is initiated by the SNS. Both divisions of the nervous system are necessary. The key is balance between the two.
Researchers, scientists, and practitioners alike speak of "vagal tone," but what is that exactly? In short, it's the strength of your vagus response. Think of vagal tone like you would muscle tone: not enough, and the nerve is soft and weak; too much, and it's tight, spasming, and cramping. The goal, of course, is somewhere in the middle. Typically, with the vagus nerve, problems arise from a low or weak tone. It may still be working, but not efficiently. When the vagal tone is too low, the nerve can't do its job to counterbalance the sympathetic response, resulting in always-on stress.
Holistic Health Applications
It would take a book (and a thick one at that!) to discuss all the ways the vagus nerve influences your health. Stress management is an obvious application, and we'll get to that shortly. But first, let's explore some other roles of the vagus nerve.
Supporting the Brain-Gut Axis
The bidirectional communication between the brain and the gastrointestinal tract, known as the "brain-gut axis," is based on a complex system, which includes the vagus nerve, the sympathetic nervous system, endocrine, immune, enteric, and humoral systems as well as the influence of gut microbiota in order to regulate gastrointestinal health and connect emotional and cognitive areas of the brain with gut functions.5,8
The vagus nerve is mostly afferent fibers, including sensations from the gut. Yet it also has efferent control over blood flow to the digestive tract, so poor vagal tone can reduce blood flow to this area, which, in turn, can cause pain due to a lack of nutrients and oxygen coming in as well as a lack of toxins going out. Digestion may also be compromised.8
The gut is an important control center of the immune system, and the vagus nerve has immunomodulatory properties as well.7 Experts estimate that 80% of immune power resides in the gut. So not only would you be at risk for poor digestion with meager vagal tone, but you could also have a compromised immune system.
Additionally, the vagus nerve interacts synergistically with hormones and peptides to regulate food intake and appetite, and it is becoming increasingly important as a therapeutic focus for gastrointestinal and psychiatric disorders, such as inflammatory bowel disease (IBD),6 depression,14 and posttraumatic stress disorder (PTSD).3 The bottom line: this nerve plays important roles in the relationship between the gut, the brain, and inflammation.4
Reducing Inflammation and Inflammatory Disease
Inflammation and its resolution play a key role in a wide variety of diseases ranging from autoimmune conditions like irritable bowel disease and multiple sclerosis to cardiovascular disease, dementia, and even aging. So, science that shows stimulating the vagus nerve can actually reduce inflammation and its associated symptoms is a critically important finding.
According to a report in Psychology Today,2 a higher vagal tone is linked to physical and psychological well-being. Conversely, a low vagal tone is associated with inflammation, depression, negative moods, heart attacks, and stroke. In 2016, an international team of researchers reported that stimulating the vagus nerve reduced pro-inflammatory cytokine levels and inflammation in subjects with rheumatoid arthritis.9 Referring to the 2016 international study, Kevin Tracey, president and CEO of the Feinstein Institute for Medical Research and the person who discovered the inflammatory reflex, stated, "…I believe this study will change the way we see modern medicine, helping us understand that our nerves can, with a little help, make the drugs that we need to help our body heal itself." 2
Reducing Stress and Anxiety
During a state of danger, stress, or excitement, your SNS sounds alarm bells all over your body, indicating something is wrong, and you need to prepare for battle. These warnings send your brain and body into survival mode, releasing the neurotransmitter epinephrine (adrenaline), which primes you to react quickly and forcefully. When the threat has passed, your brain sends signals through the vagus nerve to release the neurotransmitter acetylcholine to relax the tension.
However, the sympathetic fight-or-flight response doesn't know the difference between immediate danger and life stressors that come at us every day. In decades or even centuries past, we tended to face many more physical dangers than we do today. Now, your fight-or-flight reaction is activated not only during dangerous situations — like when you think you hear a burglar in your house — but also by more emotionally charged threats, like a difficult relationship or a job you don't enjoy.
Complicating matters, unlike the physical dangers that come and go, these contemporary threats remain part of our daily lives. And so do the stress and anxiety that can accompany them, courtesy of our fight-or-flight response.
If your PNS doesn't counteract your stress reaction, you may end up living in a constant state of anxiety, putting you at a higher risk for other health problems, such as high blood pressure, heart disease, autoimmune conditions, and Type 2 diabetes. Thankfully, this is where the vagus nerve shines. A healthy vagus nerve can rapidly offset your body's stress response. It can help reduce anxiety and improve your overall health if you know how to care for it and keep it in good working order.12
How to Improve Vagal Tone
As you can see, ensuring a well-functioning vagus nerve has the potential to improve many areas of health. In some cases, researchers have found that implanting electrical devices to stimulate the vagus nerve helps resolve profound health conditions. However, we can stimulate the vagus nerve by noninvasive means as well. In addition to the foundational practices of sound nutrition, proper exercise, enough sleep, and adequate hydration, here are a few targeted strategies we can use to support vagal nerve health.
Massage
The vagus nerve is vulnerable at certain places, particularly at the locations where it enters different body cavities, for example (1) at the base of the skull on both sides where the skull joins the cervical spine; (2) on the sides of the neck behind the angle of the jaw, at the level of cervical vertebra 1; (3) just above the medial end of the clavicle on both sides; and (4) behind the sternum where the nerve enters the stomach at the top of the abdomen. The vagus can get twisted, turned, or kinked in these locations, which results in poor blood flow and, in turn, compromises nerve tone. The good news? These four areas can benefit from manual massage.8
Tight tissue affects how well things move, especially fluid in arteries, veins, and cerebrospinal fluid, disrupting how nerves function. Nerves like to slide and glide, and they need a constant supply of nutrients as well as continual removal of waste products. The goal, therefore, is to keep tissue around nerves pliable and flexible since too much pressure on them can result in pain, numbness, or tingling. The vagus is surrounded by its own blood and lymph flow, but that supply can be compromised by surrounding tight tissues.8
Other vagus nerve therapies may not be enough to address poor vagal tone if the surrounding tissue is tight. So, consider addressing tight tissue in these four vulnerable areas first to maximize the effectiveness of other strategies.8
· Start with massaging the back of the head and back of the skull. Tightness in this area can negatively impact the vagus nerve and choke off blood supply to the brain.
· Move to massage the area on the sides of the neck behind the angle of the jaw.
· Then, massage the subclavius muscle directly underneath the clavicle (collarbone).
· Finally, follow the sternum down to its tip, at the top of the rectus abdominus muscle. Rub underneath the rib cage into the muscle on both sides, paying extra attention to the left, where the esophagus enters the stomach.
Humming or Chanting
Researchers have found that humming or chanting can be very good for the vagus nerve. These practices vibrate and stimulate your pharynx, larynx, throat, mouth, tongue, and sternum – all of which are influenced by the vagus nerve. Dr. Peter Levine, an expert in trauma and somatic healing, found that making a long "voo" sound in a deep vocal register stimulates the vagus nerve and the PNS, thus relaxing the body.16 An extended deep "hum" or "ohm" sound can do the same. Those sounds also encourage a long exhale, and long exhales increase PNS activity, thus initiating relaxation. In contrast, inhalations drive SNS activity. Hyperventilation (many short, choppy inhalations) overexcites the sympathetic stress response. So, to increase relaxation, try humming or chanting with long, slow exhales to stimulate parasympathetic activity.
The Right Kind of Exercise
Yoga, Tai Chi, and qigong are effective ways to restore vagal tone due to how nerves are stimulated through the different positions during these practices and their emphasis on calm breathing and relaxation.
When beginning a program, consider exercising with a friend, a trainer, or in a class. Not for the social interaction per se but more for the emotional support. When movement isn't typically a big part of your day, adding this into your life can be stressful. If you get sore or are unsure of what you're doing, that's even more stressful, so having a partner or guide is comforting. The goal is always less stress, not more.8
Speaking of less stress, unless you need the stability gained from holding your breath for a difficult movement, you should be able to breathe while moving. If an exercise is too challenging to breathe through, then it's too hard for the purpose of improving vagal tone. You should be able to breathe in and out normally through your nose. If you can't, that means you're too far into the stress response to be beneficial for your nervous system, and you should ease up.8
Lastly, before selecting an exercise program, it's always a good idea to talk to your healthcare provider to determine if it's safe for you.
Controlled Breathing
There are many controlled breathing techniques that can improve vagal tone. Functional medicine practitioner Dr. Andrew Weil developed one of the most straightforward strategies - the 4-7-8 breathing technique - based on breath control methods used in the pranayama yoga tradition.15 Researchers have found its therapeutic properties beneficial for many situations, including pain during childbirth1 or after surgery.13 It's also useful for releasing tension and supporting focus before or during creative expression.11
How to do it (or watch this instructional video):
- Sit comfortably with your back supported. Place your tongue where your gums meet your upper front teeth and keep it there throughout the exercise.
- Start by exhaling completely, making a "woosh" sound.
- For four seconds, inhale quietly through your nose, focusing on breathing from the diaphragm rather than the chest.
- Hold your breath for seven seconds.
- Exhale audibly through rounded lips, holding for eight seconds.
- This is one round.
The essential point of this type of breathing is to exhale twice as long as you inhale. Weil recommends beginning with four rounds to feel a shift and then adding more if you wish as you gain experience with the practice.
You Can Be Stressed Out, or You Can Heal, but Not Both
Science tells us you can't heal in survival mode. Rest or growth mode is where healing happens. Recovery is simply not a biological priority when you feel like you're fighting for your life, literally or metaphorically. Thus, being stuck in a state of sympathetic dominance (fight-or-flight) greatly reduces your chances of achieving holistic health. Your body doesn't have the biochemical supply chain required to recover when you're stressed out.10 Unfortunately, life will always be full of challenges. However, the key to stress resilience is to complete the stress cycle, i.e., return to a rest-and-digest state as quickly as possible.
The holidays are a stressful time for many, and they're right around the corner. So, keep these strategies in mind the next time you need to reduce the effects of stress or recover from anything, such as an injury or an illness. Remember to start by finding calm, and one of the best ways to do that is by stimulating the vagus nerve. As we've seen, improving vagal tone offers many health benefits on its own, but it can also be a strong foundation for increasing the effectiveness of other therapies since it "sets the stage" for healing to occur.
REFERENCES
1. Adam, et al. (2017). The Effectiveness of Deep Breathing Relaxation Technique and 4-7-8 Method Against Intensity Pain During First Active Phase of Normal Delivery at Maternity Clinics in North Sulawesi. Proceeding Manado Health Polytechnic 1st International Conference (ORAL). Vol. 1, No. 1, https://ejurnal.poltekkes-manado.ac.id/index.php/prd/article/view/373.
2. Bergland, C. (July 6, 2016). Vagus Nerve Stimulation Dramatically Reduces Inflammation: Stimulating the Vagus Nerve Reduces Inflammation and the Symptoms of Arthritis. Psychology Today, https://www.psychologytoday.com/us/blog/the-athletes-way/201607/vagus-nerve-stimulation-dramatically-reduces-inflammation.
3. Bremner, J.D., et al. (2021). Transcutaneous Cervical Vagal Nerve Stimulation in Patients with Posttraumatic Stress Disorder (PTSD): A Pilot Study of Effects on PTSD Symptoms and Interleukin-6 Response to Stress. Journal of Affective Disorders Reports, Volume 6, https://doi.org/10.1016/j.jadr.2021.100190.
4. Breit, S., et al. (March 13, 2018). Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, Vol. 9, https://doi.org/10.3389/fpsyt.2018.00044.
5. Carabotti M., et al. (2015). The Gut-Brain Axis: Interactions Between Enteric Microbiota, Central, and Enteric Nervous Systems. Annals of Gastroenterology, 28:203–209.
6. Fornaro, R., et al. (2022). Inflammatory Bowel Disease: Role of Vagus Nerve Stimulation. Journal of Clinical Medicine, 11(19):5690. DOI: 10.3390/jcm11195690.
7. Goverse, G., et al. (2016). The Intestinal Cholinergic Anti-Inflammatory Pathway. The Journal of Physiology, https://doi.org/10.1113/JP271537.
8. Healthpath (2022). Healing the Vagus Nerve with Dr. Perry Nickelston, downloaded August 28, 2023, https://www.youtube.com/watch?v=DfFCT2emwwQ.
9. Koopman, F.A., et al. (2016). Vagus Nerve Stimulation Inhibits Cytokine Production and Attenuates Disease Severity in Rheumatoid Arthritis. PNAS (Proceedings of the National Academy of Sciences of the United States of America), 113(29): 8284-8289. https://doi.org/10.1073/pnas.1605635113.
10. Lipton, B. (May 19, 2021). How Stress Affects the Body and Mind. Keto Kamp. Downloaded September 11, 2023, https://www.youtube.com/watch?v=IZ3KwN8Tpek.
11. McNair, D. (2020). Flipping on the Creative Switch Using the 4, 7, 8 Breathing Technique. The Creativity Workbook for Coaches and Creatives. Routledge,
12. (n.a.) (April 20, 2023). Your Vagus Nerve May Be Key to Fighting Anxiety and Stress. Cleveland Clinic Health Essentials. Downloaded September 2, 2023, https://health.clevelandclinic.org/what-does-the-vagus-nerve-do/.
13. Nowicki, L.V. (2021). The Effect of a Breathing Technique on Reducing Postoperative Orthopedic Pain. Doctoral Dissertation for Grand Canyon University, https://www.proquest.com/openview/6fa1e8f99e08c4535bdfcbc3c9e17d46/1?pq-origsite=gscholar&cbl=18750&diss=y.
14. Tan, C., et al. (2022). Recognizing the Role of the Vagus Nerve in Depression from the Microbiota-Gut Brain Axis. Frontiers in Neurology, DOI: 10.3389/fneur.2022.1015175.
15. Weil, A. (2014). How to Perform the 4-7-8 Breathing Exercise, Downloaded September 10, 2023, https://www.youtube.com/watch?v=YRPh_GaiL8s.
16. Winter, E. (May 2023). The Power of "Voo": Vagus Nerve Exercise for Overwhelm. Downloaded September 10, 2023, https://www.youtube.com/watch?v=oYOKFi4m-ic.
ABOUT THE AUTHOR:
 Victoria L. Freeman, Ph.D., CHFS, CMH, CBC, has traveled a long and winding professional road that includes working as a teenage fine artist, later a personal trainer and wellness coach, a college professor and administrator in exercise science and education, a freelance natural health and fitness writer for national magazines, a property manager and interior designer for vacation and executive rental properties and most recently returning to the natural health arena while attending Trinity School of Natural Health to become a Certified Holistic Fitness Specialist, a Certified Master Herbalist, and a Certified Biblical Coach.
Victoria L. Freeman, Ph.D., CHFS, CMH, CBC, has traveled a long and winding professional road that includes working as a teenage fine artist, later a personal trainer and wellness coach, a college professor and administrator in exercise science and education, a freelance natural health and fitness writer for national magazines, a property manager and interior designer for vacation and executive rental properties and most recently returning to the natural health arena while attending Trinity School of Natural Health to become a Certified Holistic Fitness Specialist, a Certified Master Herbalist, and a Certified Biblical Coach.

